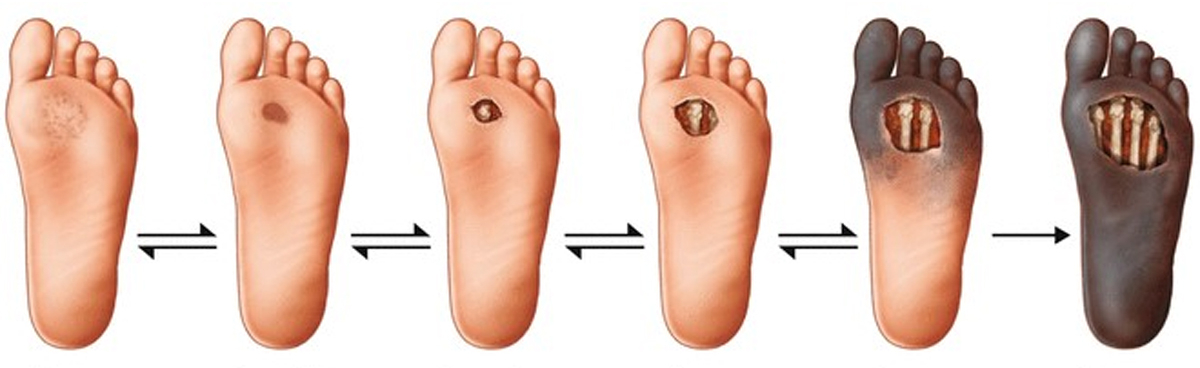
Diabetic foot surgery is a process involving the surgical treatment of serious complications in the feet of diabetic patients, such as wounds, ulcers, infections, and tissue necrosis. These surgical procedures aim to control infection, promote wound healing, and preserve foot health.
Common Procedures in Diabetic Foot Surgery
Debridement (Wound Cleaning): Removal of infected tissues from the wound to prevent infection spread and accelerate healing.
Wound Care and Drainage: Application of specialized dressings on the wound surface; drainage devices may be used to reduce infection risk.
Skin Grafts: Used to cover large wound areas and support healing.
Osteotomy: Bone adjustments to correct foot deformities and reduce pressure points.
Amputation: Removal of necrotic and infected tissues in severe infections.
Flaps (Tissue Transplant): Healthy tissues are transplanted to the wound site to promote healing.
Treatment Sequence
Diabetic foot surgery requires careful planning and disciplined application. Key steps include:
Good Diabetes Control: Balancing blood sugar is critical for surgical success and healing.
Wound Care and Evaluation: Assess wound size, type, and infection status.
Radiological Imaging: X-ray, MRI, or CT to detect bone infections and necrosis.
Debridement: Removal of necrotic tissues before surgery to clean the wound.
Surgical Intervention: Customized procedures based on wound depth and size.
Healing and Rehabilitation: Regular follow-ups to support healing and monitor infection risk.
Postoperative Recovery in Diabetic Foot Surgery
Infection Control: Antibiotic treatment may be necessary after surgery.
Wound Care: Regular dressing changes and hygiene maintenance.
Diabetes Management: Blood sugar control and dietary adjustments accelerate recovery.
Physical Rehabilitation: Physical therapy may be needed to maintain foot health and improve mobility.
Multidisciplinary Importance of Diabetic Foot Surgery
This process requires collaboration among multiple specialties:
Surgeon: Plans and performs surgical procedures.
Endocrinologist: Manages diabetes control.
Infectious Disease Specialist: Oversees infection management.
Physiotherapist: Manages rehabilitation.
Diabetic Charcot Disease
A serious condition seen in long-term diabetic patients involving nerve damage (diabetic neuropathy) that causes open wounds and bone deformities in the foot. Without early diagnosis and proper treatment, it can lead to limb loss. Nerve damage causes numbness leading to open wounds and bone weakness causing fractures and deformities.
Early symptoms include redness, swelling, and increased warmth in the foot. As neuropathy worsens, pain diminishes. Disease progression causes skin ulcers, bone protrusions, and joint abnormalities disrupting the foot’s anatomy and function.
Diagnosis is often made through patient history and physical examination; early signs may be mistaken for infection. Diagnosis is generally confirmed with X-rays.
Treatment of Diabetic Charcot Disease
Regardless of disease stage, the goal is to prevent soft tissue damage and bone deformities and achieve a stable, properly aligned foot at the end of treatment. Initial treatment involves total contact casting and offloading the foot, renewed every 2 weeks, avoiding weight bearing.
If open wounds and bone deformities develop despite treatment, surgery involving bone removal (osteotomy) and fixation of deformities may be necessary. Surgery aims to correct deformities and stabilize the foot.
Modern Adjunctive Treatments for Diabetic Foot Wounds
Adjunctive Debridement Methods
Versajet: A high-pressure water jet technique for wound debridement.
Provides clearer separation between necrotic and viable tissue.
Rapidly removes dead tissue from the wound.
Prepares wound bed and granulation tissue for faster skin grafting.
Shortens hospital stay.
Modern Wound Care Techniques and Products
There is no standard approach for diabetic wounds; care must be individualized.
VAC (Vacuum-Assisted Closure)
Prepares the wound bed, accelerates healing.
Reduces edema.
Increases granulation tissue formation and perfusion.
Removes exudate and infectious material.
EGF (Epidermal Growth Factor)
Shown to accelerate healing and reduce ulcer size in non-healing diabetic foot ulcers.
Decreases risk of recurrent lesions and hospital stay length.
Increasingly used in topical and intralesional forms.
Can be applied twice weekly.